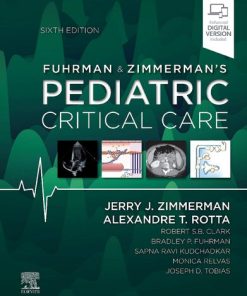
Fuhrman and Zimmerman’s Pediatric Critical Care 6th Edition by Jerry Zimmerman, Alexandre Rotta 0323672719 9780323672719
$50.00 Original price was: $50.00.$25.00Current price is: $25.00.
Fuhrman & Zimmerman’s Pediatric Critical Care 6th Edition by Jerry J. Zimmerman, Alexandre T. Rotta – Ebook PDF Instant Download/DeliveryISBN: 0323672719, 9780323672719
Full download Fuhrman & Zimmerman’s Pediatric Critical Care 6th Edition after payment.
Product details:
ISBN-10 : 0323672719
ISBN-13 : 9780323672719
Author : Jerry J. Zimmerman, Alexandre T. Rotta
In the highly specialized field of caring for children in the PICU, Fuhrman and Zimmerman’s Pediatric Critical Care is the definitive reference for all members of the pediatric intensive care team. Drs. Jerry J. Zimmerman and Alexandre T. Rotta, along with an expert team of editors and contributors from around the world, have carefully updated the 6th Edition of this highly regarded text to bring you the most authoritative and useful information on today’s pediatric critical care—everything from basic science to clinical applications.
Fuhrman & Zimmerman’s Pediatric Critical Care 6th Table of contents:
Section I: Pediatric Critical Care: The Discipline
1. History of pediatric critical care medicine
Evolution of modern medicine
Anatomy and physiology
Resuscitation and ventilatory support
Contributions of specific disciplines
Early use of mechanical ventilation in neonates and children
Poliomyelitis and creation of the first intensive care units
Definitions
First pediatric intensive care units
Central role of critical care nursing
Role of pediatric anesthesiologists and pediatricians in founding pediatric critical care medicine
Growth of pediatric critical care medicine
Cost of success in pediatric critical care medicine
Around the world
High-mortality countries
Summary
Key references
References
2. High-reliability pediatric intensive care unit: Role of intensivist and team in obtaining optimal outcomes
Pediatric intensive care unit as a system
Models of critical care delivery
Summary
References
3. Critical communications in the pediatric intensive care unit
Intensive care unit design
Medical record
Huddles
Checklists
Rounds
Closed-loop communication
Transitions of care
Medical training
Debriefing
Team training
Conclusion
Key references
References
4. Professionalism in pediatric critical care
Profession
The virtuous doctor
Stakes
Great paradox of the medical profession
Professionalism, the physician charter
Pediatric intensive care unit as a site for medical education and lifelong learning
References
5. Leading and managing change in the pediatric intensive care unit
National change day: A case study in leading change
History and development of change management
Change management in healthcare
Models and tools to facilitate change leadership and management
Conclusion
Key references
References
6. Evolution of critical care nursing
Early pediatric critical care nursing
Describing what nurses do: The synergy model
Leadership
Evolution of advanced practice registered nurses into pediatric critical care
Nursing research
Summary
Key references
References
7. Fostering a learning healthcare environment in the pediatric intensive care unit
Learning healthcare system
Foundation predicated on professionalism
Pillars of a learning healthcare environment
Benefits of a learning healthcare environment
Key references
References
8. Challenges of pediatric critical care in resource-poor settings
Child mortality rates
Cost considerations in critical care delivery
Ethics of intensive care in resource-poor settings
Strengthening critical care infrastructure
Critical illness during public health emergencies
Key references
References
9. Public health emergencies and emergency mass critical care
How many pediatric patients could be affected in a public health emergency?
What are the most likely public health emergencies?
Who will make decisions during an emergency?
What is the expected timeline of a public health emergency?
What is a surge and what can be done to meet surge needs?
How can the intensive care unit support the emergency department during a public health emergency?
How can all intensive care units work together?
What steps can be taken to maximize intensive care unit treatment in a disaster?
How will the intensive care unit evacuate if needed?
How should pediatric patients be tracked?
How will limited services be ethically rationed?
What are the mental health considerations relevant to emergency mass critical care?
What is the role of medical learners in public health emergencies?
Conclusion
Key references
References
10. Lifelong learning in pediatric critical care
Adult learning theory in medical education
Graduate medical education
Accreditation council for graduate medical education core competencies, milestones, and entrustable professional activities
Beyond graduate medical education
New methods of assessment and future challenges
Key references
References
Section II: Pediatric Critical Care: Tools and Procedures
11. Essential concepts in clinical trial design and statistical analysis
Purpose of a clinical trial
Clinical trial design
Phases of clinical trials for new drug approval
Statistical analysis and reporting
Hypothesis testing and determining the study result
Conclusions
Key references
References
12. Prediction of short-term outcomes during critical illness in children
Historical perspective
Methods
Current prediction tools for assessment of mortality risk
Next generation: Morbidity and mortality prediction—trichotomous outcome
Future directions: Predictive analytics and tools for decision support
Key references
References
13. Pediatric critical care transport
Pediatric transport systems
Components of a specialized interfacility transport team
Referring hospital responsibilities
Summary
Key references
References
14. Pediatric vascular access and centeses
Intraosseous infusion
Arterial catheter placement
Central venous line placement
Peripherally inserted central venous catheters
Umbilical arterial catheter and umbilical venous catheter placement
Thoracentesis
Tube thoracostomy
Pericardiocentesis
Abdominal paracentesis
Key references
References
15. Ultrasonography in the pediatric intensive care unit
Ultrasound physics and basics of image optimization
Procedural guidance
Drainage procedures
Lumbar puncture
Diagnostic modalities
Translation to practice
Conclusion
Key references
References
Section III: Pediatric Critical Care: Psychosocial and Societal
16. Patient- and family-centered care in the pediatric intensive care unit
Definition of “family”
Historical evolution of patient- and family-centered care
Fundamental needs of patients and families in the intensive care unit
Core principles of patient- and family-centered care1,12
Patient- and family-centered care improves outcomes for all stakeholders
Overcoming barriers and challenges to patient- and family-centered care in the intensive care unit
Summary
Key references
References
17. Pediatric critical care ethics
Defining bioethics
Approach to bioethics dilemmas in the pediatric intensive care unit
Ethics of patient and surrogate decision-making
Other ethical issues in the pediatric intensive care unit
Goals for the ethical practice of the intensivist
Key references
References
18. Ethical issues around death and dying
Decision-making at the end of life
Requests for potentially inappropriate treatments in the intensive care unit
Withholding and withdrawing of life-sustaining treatments
Administration of analgesics and sedatives in end-of-life care
Is there a role for neuromuscular blockade in end-of-life care?
Artificial hydration and nutrition
Key references
References
19. Palliative care in the pediatric intensive care unit
Palliative care consults in the pediatric intensive care unit
Communication
Limitation of interventions
Pain and symptom management
Care of family and staff after a child’s death
Key references
References
20. Organ donation process and management of the organ donor
Process of organ donation
Determination of neurologic death
Brain death physiology
Pediatric donor management
Treatment of hemodynamic instability
Hormonal replacement therapy
Management of pulmonary issues for the potential pediatric organ donor
Fluid and electrolyte disturbances
Diabetes insipidus
Oliguria
Medical examiner and coroner issues and organ donation for children
Donation after circulatory death
Contraindications to organ donation
Evolving areas of transplantation
Summary
Key references
References
21. Long-term outcomes following critical illness in children
Post–intensive care syndrome
Health-related quality of life
Assessing change from baseline
Summary of outcomes in general pediatric intensive care unit populations
Outcomes for common pediatric intensive care unit illness categories
Examples of postdischarge outcomes in pediatric interventional trials
Strategies to assess long-term outcomes
Potential targets for interventions
Conclusion
Key references
References
22. Burnout and resiliency
Burnout and compassion fatigue in pediatric critical care providers
Critical care societies work to address burnout
Strategies for building resilience
Promoting a healthy work environment
Summary
Key references
References
Section IV: Pediatric Critical Care: Cardiovascular
23. Structure and function of the heart
Anatomic development and structure
Physiologic development and function
Key references
References
24. Regional peripheral circulation
General features
Regional circulations
Conflicting needs of regional circulations
Key references
References
25. Endothelium and endotheliopathy
Normal endothelial function
Endothelial cell dysfunction
Biomarkers of endothelial activation
Conclusions
Key references
References
26. Principles of invasive cardiovascular monitoring
Role of invasive hemodynamic monitoring
Indications for invasive hemodynamic measurements
Principles of measurement
Invasive techniques
Monitoring techniques with the pulmonary artery catheter
Catheter placement
Measurement of cardiac output
Calculation of oxygen delivery and consumption
Novel monitoring strategies
Conclusions
Key references
References
27. Assessment of cardiovascular function
Cardiovascular function
Quantity of therapy
Variables that determine tissue oxygenation
Monitoring tissue oxygenation
Assessing variables that affect the quantity of therapy
Physiology of the patient with a single ventricle
Key references
References
28. Cardiac failure and ventricular assist devices
Pediatric heart failure
Mechanical circulatory support in pediatric patients
Extracorporeal life support
Ventricular assist devices
Indications and management
Basic management of ventricular assist device patients
Ventricular assist device—congenital heart disease and single-ventricle physiology
Outcomes
Current perspective and future directions
Conclusions
Key references
References
29. Echocardiographic imaging
Components of the examination
Modalities
Structural congenital heart disease and intracardiac shunting
Valve anatomy and function
Ventricular function
Pulmonary hypertension
Pericardial effusion
Intracardiac vegetations and thrombi
Kawasaki disease and coronary artery anomalies
Intravascular catheters
Balloon atrial septostomy
Extracorporeal membrane oxygenation and ventricular assist devices
Key references
References
30. Diagnostic and therapeutic cardiac catheterization
Catheterization laboratory environment
Diagnostic cardiac catheterization
Therapeutic cardiac catheterization
Risks and complications
Cardiac catheterization and extracorporeal membrane oxygenation
Conclusion
Key references
References
31. Pharmacology of the cardiovascular system
Mechanisms of response
Sympathomimetic amines
Bipyridines
Digitalis glycosides
Conclusion
Key references
References
32. Cardiopulmonary interactions
Effects of ventilation on circulation
Effects of cardiovascular function on respiration
Key references
References
33. Disorders of cardiac rhythm
Classification of arrhythmias
Approach to diagnosis
Treatment of rhythm disturbances
Approach to therapy
Specific arrhythmias
Key references
References
34. Shock states
Definition and physiology
Functional classification and common underlying etiologies
Multisystem effects of shock
Monitoring
Treatment
Specific shock state therapy considerations
Other therapies
Summary
Key references
References
35. Pediatric cardiopulmonary bypass
Background
Equipment and preparation for cardiopulmonary bypass
Cardiopulmonary bypass
Key references
References
36. Critical care after surgery for congenital cardiac disease
Neonatal considerations
Preoperative care
Postoperative care
Critical care management of selected specific lesions
Summary
Key references
References
37. Cardiac transplantation
Background
Indications for transplant
Transplant evaluation
Transplant listing
Management of the potential heart transplant recipient
Critical care management of the orthotopic heart transplant recipient
Complications of immunosuppression in heart transplant recipients that occur in the pediatric intensive care unit
Future management strategies for critical care of infants and children with cardiopulmonary failure
Key references
References
38. Physiologic foundations of cardiopulmonary resuscitation
Mechanisms of blood flow
Rate and duty cycle
Newer cardiopulmonary resuscitation techniques
Pharmacology
Management of ventricular fibrillation
Future directions
Key references
References
39. Performance of cardiopulmonary resuscitation in infants and children
Four phases of cardiac arrest
Epidemiology of pediatric cardiac arrest
Optimizing blood flow during cardiopulmonary resuscitation
Pediatric cardiopulmonary resuscitation targets
Airway and breathing management during cardiopulmonary resuscitation
Physiologic targets
Medications used to treat cardiac arrest
Postarrest interventions
Other considerations
Controversies in pediatric cardiac arrest management
Summary
Key references
References
Section V: Pediatric Critical Care: Pulmonary
40. Structure and development of the upper respiratory system
Developmental anatomy of the upper airway
Anatomy and physiology of the upper airway
Key references
41. Structure and development of the lower respiratory system
Lower respiratory system
Lung circulation
Summary
Key references
References
42. Physiology of the respiratory system
Physiology of the respiratory system
Gas exchange
Key references
References
43. Noninvasive respiratory monitoring and assessment of gas exchange
Pulse oximetry
Principles of pulse oximetry
Validation
Sources of error
Probe placement
Tissue oximetry
Near-infrared spectroscopy
Capnometry and capnography
Operating principles of capnometry
Physiologic basis
Differential diagnosis of abnormal capnograms
Clinical applications
Transcutaneous monitoring
Oxygen monitoring
Carbon dioxide monitoring
Conclusion
Key references
References
44. Overview of breathing failure
Physiology of breathing
Controls of breathing
Breathing failure
Conclusion
Key references
References
45. Ventilation/perfusion inequality
Distribution of ventilation
Distribution of perfusion
Fractal model of pulmonary blood flow and ventilation
VA/Q abnormalities in pulmonary disease
Therapeutic considerations
Key references
References
46. Mechanical dysfunction of the respiratory system
Pump dysfunction and failure
Therapeutic maneuvers to improve mechanical dysfunction of the respiratory system
Key references
References
47. Diseases of the upper respiratory tract
Anatomy and physiology
Diagnosis and management
Congenital malformations of the upper airway
Neoplasms of upper airway disease
Croup
Epiglottitis
Bacterial tracheitis
Peritonsillar abscess
Retropharyngeal abscess
Iatrogenic and acquired disorders of the upper airway
Pediatric tracheostomy
Foreign body aspiration
Burn injury to the upper airway
Airway trauma
Key references
References
48. Pediatric acute respiratory distress syndrome and ventilator-associated lung injury
Clinical features: Pathophysiology
Definition
Epidemiology
Pathobiology
Ventilator management
Ventilator-associated lung injury
Extracorporeal life support
Key references
References
49. Acute viral bronchiolitis
Microbiology
Epidemiology and risk factors
Pathophysiology
Clinical features and diagnosis
Prevention
Treatment
Complications
Key references
References
50. Asthma
Epidemiology and risk factors
Pathophysiology
Clinical assessment
Laboratory data
Electrocardiography
Spirometry
Treatment
Management in the intensive care unit
Mechanical ventilation
Antibiotics
Bronchoscopy
Extracorporeal life support
Prognosis
Key references
References
51. Neonatal pulmonary disease
Acute respiratory disorders
Immature respiratory control
Pulmonary malformations
Nonpulmonary causes of respiratory distress
Neonatal chronic lung disease of prematurity: Bronchopulmonary dysplasia
Key references
References
52. Pneumonitis and interstitial disease
Pathogenesis
Pathophysiology
Diagnosis
Bacterial pneumonitis
Viral pneumonitis
Fungal pneumonitis
Primary pulmonary fungi
Opportunistic pulmonary mycoses
Pneumocystis jirovecii pneumonia
Chemical pneumonitis
Idiopathic interstitial lung disease
Pediatric pulmonary hemorrhage
Summary
Key references
References
53. Diseases of the pulmonary circulation
Definition and classification
Pathology of pulmonary hypertension
Diagnostic evaluation of pulmonary hypertension/pulmonary vascular disease
Pharmacotherapy
Pulmonary hypertension in the context of specific diseases
Acute pulmonary hypertension crisis/right ventricular failure
Right ventricular dysfunction in pulmonary hypertension
Recent advances in molecular mechanisms and novel therapeutic targets in pulmonary hypertension
Long-term outcomes of patients with pulmonary vascular disease
Future directions and perspectives
Key references
References
54. Mechanical ventilation and respiratory care
Applied respiratory physiology
Indications for mechanical ventilation
Design and functional characteristics of ventilators
Ventilation for selected underlying pathophysiology
Patient-ventilator asynchrony
High-frequency ventilation
Adverse effects of mechanical ventilation
Specialty gases
Respiratory care during mechanical ventilation
Weaning from mechanical ventilation and extubation
Key references
References
55. Noninvasive ventilation in the pediatric intensive care unit
Epidemiology
Physiology and application of noninvasive ventilation
Patient selection
Patient monitoring and complications
Sedation during noninvasive ventilation
Failure of noninvasive ventilation
Long-term use of noninvasive ventilation
Key references
References
56. Extracorporeal life support
A trip around the extracorporeal membrane oxygenation circuit
Patient populations treated with extracorporeal life support
Patient selection criteria
Physiology of extracorporeal life support: Gas exchange and oxygen delivery
Patient management on extracorporeal membrane oxygenation
Weaning from extracorporeal membrane oxygenation
Complications from extracorporeal membrane oxygenation
Outcomes from extracorporeal life support
Future of extracorporeal membrane oxygenation
Key references
References
57. Pediatric lung transplantation
Indications
Contraindications
Survival and outcomes
Evaluation of the donor
Surgical approach
Presurgical management in the intensive care unit
Postsurgical management
Immunosuppression
Immunobiology
Rejection
Chronic lung allograft dysfunction
Summary
Key references
References
Section VI: Pediatric Critical Care: Neurologic
58. Structure, function, and development of the nervous system
Major cell types
Intercellular communication in the nervous system
Neurotransmitter systems
Major anatomic organization of the nervous system
Blood-brain barrier
Ventricles and cerebrospinal fluid
Vasculature in the central nervous system
Emerging characterization of the “lymphatic” circulation in the central nervous system
Developmental processes relevant to pediatric critical care medicine
New insights in neurodevelopment relevant to pediatric critical care
Conclusion
Key references
References
59. Critical care considerations for common neurosurgical conditions
Hydrocephalus
Arachnoid cysts
Chiari malformations
Dandy-walker complex
Encephalocele and meningocele
Conclusions
Key references
References
60. Neurologic assessment and monitoring
Nursing role in the recognition of neurologic complications of critical illness
Anticipatory planning for new neurologic deficits
History and assessment of risk factors
Iatrogenic complications of pharmacotherapy
Vital signs
General physical exam
Importance of observation in the neurologic exam
Assessment of level of consciousness and mental status
Fundoscopic examination
Cranial nerve examination
Approach to the motor exam
Reflexes
Cerebellar function and gait evaluation
Sensory examination
Abnormal movements or altered sensorium in the child with static encephalopathy
Distinguishing functional deficits from nonorganic pathology in the pediatric intensive care unit
Goals of the neurologic examination in the pediatric intensive care unit
Neuroimaging
Integrating neurologic monitoring data
Key references
References
61. Neuroimaging
Imaging modality overview
Hypoxic ischemic injury and germinal matrix hemorrhage in the neonate
Imaging of neurovascular disorders
Intracranial hemorrhage and vascular malformations
Central nervous system infection
Demyelinating disease
Trauma
Hydrocephalus
Tumor
Seizures
Conclusion
Key references
References
62. Coma and depressed sensorium
Definitions
Epidemiology
Relevance
Physiology/pathophysiology
Etiology
Initial treatment of the comatose child
History
Physical examination
Herniation syndromes
Diagnostic evaluation
Treatment goals: Initial and ongoing
Prognosis and outcomes
Key references
References
63. Intracranial hypertension and monitoring
Clinical background
Physiology of the intracranial vault
Measurement of intracranial pressure
Clinical analysis of intracranial pressure
Supplementing intracranial pressure monitoring with other monitoring modalities
Mechanism of brain injury in intracranial hypertension
Intracranial pressure monitoring and the postinsult natural history of injury
Key references
References
64. Status epilepticus
Definition of status epilepticus
Outcome of status epilepticus
Status epilepticus classification
Seizure types and classification
Seizures in the pediatric intensive care unit
Posttraumatic epilepsy
First- and second-line pharmacotherapy
Management of refractory status epilepticus and other forms of treatment-resistant status epilepticus
Surgical options
Changing goals of therapy in prolonged SRSE/FIRES
Key references
References
65. Hypoxic-ischemic encephalopathy
Epidemiology
Mechanisms of hypoxic-ischemic brain injury
Clinical pathophysiology
Clinical outcome and prognostication after pediatric cardiac arrest
Response of the immature brain to cardiac arrest
Treatment after cardiac arrest
Current and novel therapies and interventions
Futuristic approaches
Summary
Key references
References
66. Pediatric stroke and intracerebral hemorrhage
Significance
Arterial ischemic stroke
Etiologies and risk factors
Pathophysiology
Presentation
Neuroimaging
Laboratory evaluation
Treatment
Cerebral sinus venous thrombosis
Spontaneous intracranial hemorrhage
General care of the child with intracerebral hemorrhage
Conclusion
Key references
References
67. Central nervous system infections and related conditions
Bacterial meningitis
Subdural empyema
Brain abscess
Viral meningoencephalitis
Acute disseminated encephalomyelitis
Key references
References
68. Acute neuromuscular disease and disorders
Guillain-Barré syndrome
Myasthenia gravis
Congenital and transient neonatal myasthenia gravis
Tick paralysis
Periodic paralyses
Hypokalemic periodic paralysis
Hyperkalemic periodic paralysis
Botulism
Diphtheria
Acute intermittent porphyria
Spinal muscular atrophy
Poliomyelitis
Polio-like syndromes
Organophosphate and carbamate poisoning
Key references
References
69. Acute rehabilitation and early mobility in the pediatric intensive care unit
Rehabilitation team members in the pediatric intensive care unit
Important considerations for mobility in the pediatric intensive care unit
Acute rehabilitation across the intensive care unit continuum
Implementation of acute rehabilitation in the pediatric intensive care unit: Evidence and strategies
Summary
Key references
References
Section VII: Pediatric Critical Care: Renal
70. Renal structure and function
Renal anatomy
Renal development
Renal vasculature
The nephron
Tubular anatomy
Summary
Key references
References
71. Fluid and electrolyte issues in pediatric critical illness
Sodium
Hyponatremia
Hypernatremia
Potassium
Hyperkalemia
Magnesium
Hypomagnesemia
Hypermagnesemia
Calcium
Hypocalcemia
Hypercalcemia
Hypophosphatemia
Hyperphosphatemia
Key references
References
72. Acid-base disorders
Overview of acid-base physiology
Tools for interpreting acid-base disorders
Clinical approach to disorders of acid-base balance
Metabolic acidosis
Metabolic alkalosis
Respiratory acid-base derangements
Mixed acid-base derangements
Summary
Key references
References
73. Tests of kidney function in children
Assessment of glomerular function and injury
Renal clearance techniques
Plasma disappearance techniques
Renal inulin clearance compared with other glomerular filtration rate measurement techniques
Estimating equations
Neonatal renal function
Biomarkers of acute kidney injury and the next generation
Tubular function
Integration of kidney function assessment in critical care
Key references
References
74. Glomerulotubular dysfunction and acute kidney injury
Physiology of glomerular filtration
Glomerulotubular dysfunction
Treatment of acute kidney injury
Acute kidney injury: Clinical impact
Specific kidney diseases that may lead to acute kidney injury
Conclusions
Key references
References
75. Pediatric renal replacement therapy in the intensive care unit
Basic physiology of dialysis and ultrafiltration
Peritoneal dialysis
Intermittent hemodialysis
Continuous renal replacement therapy
Outcomes of renal replacement in critically ill children
Advances in pediatric renal replacement therapies
Summary
Key references
References
76. Pediatric renal transplantation
Donor source: Living donor versus deceased donor
Timing of transplantation
Histocompatibility
Surgical procedure
Posttransplantation monitoring
Recovery of renal function
Immunosuppression
Infection surveillance and prevention
Posttransplantation complications
References
77. Renal pharmacology
Kidney function and drug disposition
Drug dosing in kidney disease
Drug dosing in dialysis
Kidney as a therapeutic target: Diuretics and agents regulating renal excretion
Medications for the prevention/reversal of acute kidney injury
Key references
References
78. Acute severe hypertension
Terminology
Etiology
Pathophysiology
Endothelial homeostasis
Sympathetic nervous system activation
Renin-angiotensin-aldosterone system
Nitric oxide
Volume overload
Clinical presentation
Pharmacologic therapy
Special situations
Summary
Key references
References
Section VIII: Pediatric Critical Care: Metabolic and Endocrine
79. Cellular respiration
Pathways of cellular respiration
Impaired cellular respiration in critical illness
Clinical assessment of oxygen utilization
Lactate
Venous oxygen saturation
Microdialysis
Near-infrared spectroscopy
Optical spectroscopy
Tissue oxygen tension
Magnetic resonance spectroscopy
Blood mitochondrial DNA
Mitochondrial- and bioenergetic-targeted therapy in critical illness
Antioxidants
Glycemic control
Substrate provision
Mitochondrial biogenesis and mitophagy
Membrane stabilizers
Hibernation
Mitochondrial transplantation
Conclusions
Key references
References
80. Biology of the stress response
Definitions and background
Stress system primary elements
Stress response
Stress response in critical illness
Recommendations and conclusions
Key references
References
81. Inborn errors of metabolism
Pathophysiology of inborn errors of metabolism
Inheritance of inborn errors of metabolism
Signs and symptoms of inborn errors of metabolism
Laboratory evaluation of suspected inborn errors of metabolism
Postmortem evaluation of a child with suspected inborn errors of metabolism
Emergency treatment of children with suspected inborn errors of metabolism
Classification of inborn errors of metabolism by clinical presentation
Metabolic acidosis
Hypoglycemia
Cardiomyopathy and inborn errors of metabolism
Metabolic myopathies and rhabdomyolysis
Neonatal screening
Conclusions
Key references
References
82. Progress towards precision medicine in critical illness
Genetic variation and critical illness
Transcriptomics and critical illness
Plasma biomarkers and critical illness
Summary
Key references
References
83. Molecular foundations of cellular injury
Caspase-dependent forms of regulated cell death
Caspase-independent forms of regulated cell death
Cell death as a therapeutic target
Key references
References
84. Endocrine emergencies
Hypothalamic-pituitary-adrenal axis
Cortisol biochemistry and biology
Actions of cortisol
Assessing the cortisol stress response
Adrenal insufficiency in the intensive care unit
Corticosteroid side effects
Alterations of glucose homeostasis
Hyperglycemia
Glucose measurement
Hypoglycemia
Alterations of thyroid hormone in critical illness
Key references
References
85. Diabetic ketoacidosis
Etiology, definition, and presentation
Epidemiology
Management guidelines (fig. 85.1)
Diabetic ketoacidosis–associated complications
Healthcare costs associated with diabetic ketoacidosis
Key references
References
Section IX: Pediatric Critical Care: Hematology and Oncology
86. Structure and function of the hematopoietic organs
Normal peripheral blood values
Structure of the bone marrow
Function of the bone marrow: Hematopoiesis
Lymphopoiesis
Key references
References
87. The erythron
Oxygen transport
Carbon dioxide transport
Biophysical factors influencing gas transport
Regulation of blood flow distribution by red blood cells
Summary
Key references
References
88. Hemoglobinopathies
Globin gene loci
Sickle cell disease
Thalassemia
Key references
References
People also search for Fuhrman & Zimmerman’s Pediatric Critical Care 6th:
fuhrman & zimmerman’s pediatric critical care
fuhrman and zimmerman’s pediatric critical care
fuhrman and zimmerman
fuhrman and zimmerman’s pediatric critical care pdf
dr fuhrman sheboygan
Tags: Fuhrman, Zimmerman, Pediatric Critical, Jerry Zimmerman, Alexandre Rotta
You may also like…
Politics & Philosophy - Others
Uncategorized
Relationships & Lifestyle - Pregnancy & Childcare
Medicine - Pediatrics
Fuhrman and Zimmerman’s Pediatric Critical Care 6th Edition Jerry J. Zimmerman
Others
The Romantic Literary Lecture in Britain 1st edition by Sarah Zimmerman 0192569561 9780192569561
Medicine - Pediatrics